Frustrated by conventional advice, he realized the medical world was focused on the symptom (size), while ignoring the one system that truly matters for a man's internal 'hydraulics'.
Let me be honest with you...
Three years ago, my quality of life was suffering. Everyone thought I was doing fine. Retired, married for 35 years, two college-educated kids, a paid-off house...
But the truth? I was struggling silently.
Seven times. Every Single Night. That's how many times I was waking up to use the bathroom. Sometimes it was 8. On bad days, it reached 10. I'd go to bed at 10 PM with anxiety. Anxiety about waking up again. Anxiety about not being able to fall back asleep. Anxiety about disturbing my wife for the tenth time.
And when I finally made it to the bathroom?
A weak stream. Slow. Uncomfortable. I'd stand there at 3 AM, staring at the ceiling, thinking: "How did I get to this point?"
At 62, I woke up 7 times a night. Then I made a simple discovery:
The real issue isn't size. It's your body's internal hydraulics.
By Robert Parker* | Published October 24, 2024 | 8-minute read
*Name changed to protect privacy
⚠️ IMPORTANT DISCLAIMER - This content is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease.
Always consult your physician before starting any supplement, especially if you have medical conditions or take medications. ProstaVive is a dietary supplement not evaluated by the FDA. Individual results may vary. Testimonials do not guarantee similar results.
But the worst part wasn't the sleepless nights. The worst part was watching my wife, Maria, grow distant.
She never complained. Not once.
But I could see it in her eyes. The exhaustion. The frustration. The sadness. She started sleeping in the guest room "so I wouldn't wake her." Our marriage was quietly fading. And my social life? Forget it. Barbecue at friends' houses? I spent more time looking for the bathroom than socializing. Road trips? Had to stop every 40 minutes. Movies? Impossible. I'd leave 3 times during the film. I had become a prisoner of my own prostate concerns.
And the worst part: I was embarrassed to talk about it. Embarrassed to tell friends. Embarrassed to fully discuss with my doctor. Embarrassed even to research online.

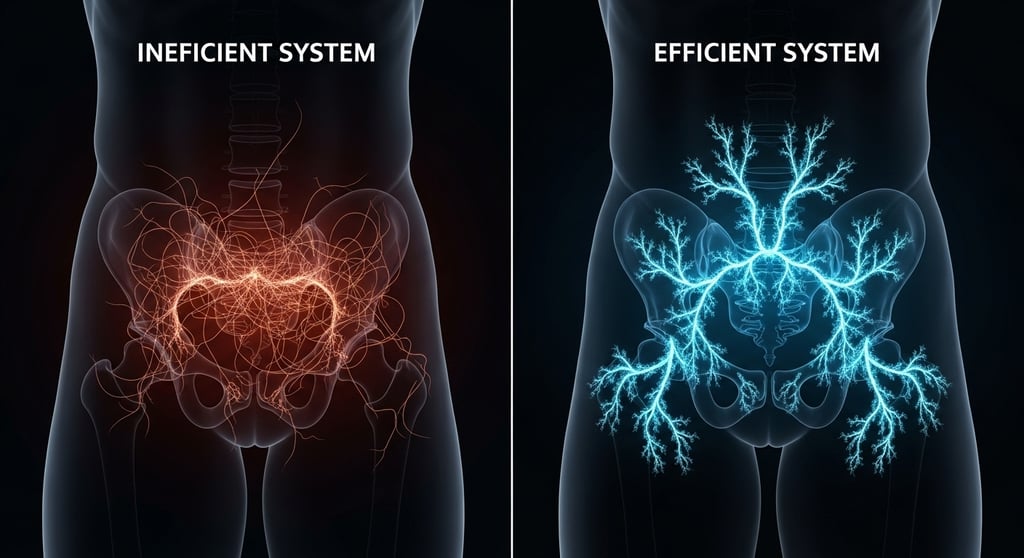
The Scientific Revelation: The Principle Behind Male “Hydraulics”
My research led me to a fascinating field of human biology. I discovered that the key to an efficient vascular system, the true basis of male “hydraulics,” revolved around a single, powerful molecule: nitric oxide. Think of it as your body's master flow controller.
The logic, just like in engineering, was irrefutable:
Efficient blood flow is the foundation of everything. Nitric Oxide is the key molecule that helps relax blood vessels, allowing for healthy circulation. Ingredients such as artichoke extract and amino acid precursors are studied for their role in supporting the body's natural production of nitric oxide.
This is not just a theory. The importance of nitric oxide for vascular function is a validated field of study, as detailed in this review article from the renowned Journal of Hypertension:
Supporting Scientific Source: “Nitric Oxide and Vascular Function: New Insights”
The evidence was clear. The most logical approach was not to attack the symptom, but to nourish the system. By supporting the natural production of nitric oxide, I would be supporting the “hydraulics” that underpin the overall well-being of the pelvic region.
This left me with one last question, the most important one of all: What is the best way to provide the body with the natural “building blocks” needed to optimize this vital system?
Putting the Puzzle Together: The Pieces That Science and Tradition Pointed To
My discovery about nitric oxide and “hydraulics” was the centerpiece of the puzzle. But a plan is nothing without the right materials. So my next phase of research was obsessive: identifying the most promising natural “building blocks” that science and history pointed to for supporting male wellness.
I wasn't looking for a “silver bullet,” but rather an elite team of nutrients that could work synergistically. My research led me to a remarkable list of 11 key components.
The “Attack Team”: 8 Components for Vitality and Flow
These were the ingredients that appeared repeatedly in studies and traditional texts on male energy, flow, and vitality.
Tongkat Ali and Panax Ginseng: I discovered that cultures in Southeast Asia and Manchuria have used these extracts for centuries to support male stamina and vigor.
Ashwagandha and Fenugreek: Modern science calls them “adaptogens.” I saw them as “system managers,” known to help the body cope with stress and maintain natural hormonal balance.
Maca Root and Artichoke Extract: These were the “protectors.” I found research on their role in antioxidant support, helping to protect cells from everyday stress.
Nettle Root and Boron: Nettle Root was the most famous of all for directly supporting healthy prostate function. Boron, a trace mineral, appeared to be an essential facilitator for many male processes.
The “Foundation”: 3 Essential Minerals
As an engineer, I know that the foundation is everything. These three minerals formed the basis on which the entire system was supposed to operate.
Zinc: Everywhere I read, zinc was described as “the man's mineral,” vital for immune support and healthy hormone balance.
Magnesium: Essential for over 300 reactions in the body, including normal muscle function and promoting a state of relaxation.
Vitamin D: I discovered that it acts almost like a hormone, being crucial for immune support and overall cellular health.
The Final Discovery: Synergy is Key
But my biggest insight was this: it wasn't just about having the right pieces. It was about how they fit together. Like a complex circuit, the proportions and combination were everything.
That's why I knew I couldn't just buy these ingredients separately. I needed a formula where experts had calibrated the dosages to create a synergistic effect, where 1 + 1 didn't equal 2, but 3. It was this search for the perfect formula that led me to ProstaVive.


The Logical Decision: Putting My Research to the Test
After weeks of research, I finally found what I was looking for: ProstaVive. It wasn't just another supplement; it was the only formula that perfectly matched the “engineering specifications” I had established:
✓ Focus on the Right Mechanism: It was designed around supporting nitric oxide flow and production, not outdated theories.
✓ Comprehensive Ingredient Matrix: It contained the key “building blocks” that my research had identified as crucial.
✓ Design for Efficiency: The powder format made logical sense for optimal absorption.
✓ Quality Assurance: Manufactured in a certified lab, which for me, as an engineer, was non-negotiable.
Still, I was skeptical. Very skeptical. But the 180-day guarantee removed the risk from the equation. It was a logical test. I could put my hypothesis to the test without risking a single penny. I thought, “Okay, let's see the data.”
The Journey: From Interrupted Nights to Freedom
The first few weeks required patience. I trusted the process, knowing that complex systems don't change overnight.
Then I started to notice the little things. That feeling of constant urgency began to subside. The flow seemed more steady. One morning, I woke up and realized I had only gotten up twice. For me, that was already a monumental step forward.
And then, about a month later, something happened that I hardly dared to hope for.
I laid my head on the pillow... and the next thing I knew, sunlight was streaming through the window. I had slept through the night. The feeling wasn't just one of rest; it was one of relief. It was as if a weight I didn't even know I was carrying had been lifted.
The Ripple Effect: How a Good Night's Sleep Changed Everything
What I didn't anticipate was the ripple effect that one restorative night's sleep would have on my entire life. It wasn't just about the bathroom; it was about getting my life back.
Energy and Clarity: The chronic fatigue disappeared. I began waking up feeling sharp and ready for the day, with the energy to play with my grandchildren and pursue my hobbies.
Confidence and Freedom: My confidence skyrocketed. We took a four-hour trip to the beach, and for the first time in years, I wasn't anxiously looking for the next rest stop. I felt in control again.
Mood and Relationship: Maria said it was like having the “old Robert” back. The tension that had built up between us because of my exhaustion and worry simply dissolved. We reconnected. She moved back into our bedroom, and our marriage is stronger than ever.
Today, 8 months later, the change is profound. It's not about numbers in a journal; it's about the quality of each day. It's about feeling like myself again.
Proof I Wasn't Alone: Real Stories from Real Men
After my own experience, I needed to know if it was just my case. I started sharing my journey with close friends, men I knew were facing similar challenges in silence.
Their response was the final confirmation that I was on the right path. Their stories are the most powerful proof I can offer.
IMPORTANT DISCLAIMER: The experiences shared below are from real users of ProstaVive. However, individual results can and will vary significantly. These stories do not represent a typical outcome and should not be interpreted as a promise or guarantee. This product is not intended to diagnose, treat, cure, or prevent any disease.
📍 CHARLES - My Fishing Buddy
Charles and I have been fishing together for years, but he had stopped coming. When I asked, he admitted he couldn't handle hours on a boat anymore and that the sleepless nights were taking a toll on his marriage. I suggested he look into the "flow support" approach I had discovered.
Six weeks later, he called me, emotional. "Robert... I had my first truly restful night's sleep in years. My wife and I talked this morning, and we felt a sense of hope we haven't felt in a long time." Today, Charles is back on the boat, and more importantly, he and his wife are reconnecting.
⭐⭐⭐⭐⭐ "My quality of life has dramatically improved"
"I was 58 and the lack of sleep was affecting everything. After adopting a new approach with ProstaVive, the quality of my sleep has noticeably improved. This has had a positive impact on my overall well-being. Thank you!"
— Charles M., 58, California | ✓ Verified Buyer
📍 JOSEPH - My Skeptical Former Colleague
Joseph, a brilliant engineer, has always been a skeptic. He told me his doctor had recommended a procedure and that it was his only option. The procedure was two months away. I simply said, "Joe, you have two months and a 180-day guarantee. What's the risk in trying a nutritional support approach first?"
He reluctantly agreed. Five weeks later, he went for his pre-op tests. His doctor was surprised by the improvement in his overall well-being and urinary comfort. Together, they decided the procedure was no longer an immediate necessity and agreed to monitor the situation. Joseph was relieved to be able to explore a less invasive option.
⭐⭐⭐⭐⭐ "We decided to postpone the procedure"
"My doctor had recommended a procedure. I decided to try ProstaVive as a supportive approach. My comfort improved so much that my doctor and I agreed to postpone the procedure indefinitely. I'm grateful for the support this supplement provided."
— Joseph A., 64, Texas | ✓ Verified Buyer
📍 ANTHONY - My Golf Partner
Anthony moved to Florida to be near his grandkids but barely saw them. The long car rides were a nightmare for him. He felt like a prisoner. I sent him a 3-month supply of ProstaVive with a note: "Look into this. Trust the process."
Two months later, I got a photo of him with his whole family at a beach hours away from his home. The text said: "The drive was so much smoother than I expected. You gave me my family back."
⭐⭐⭐⭐⭐ "Started traveling again with more comfort"
"I had stopped taking long car trips. Now, with the support of ProstaVive, I can travel to visit my family with much more comfort and less worry. It's been life-changing!"
— Anthony R., 61, Florida | ✓ Verified Buyer
📍 FRANK - My Neighbor
Frank was going through a tough time. He opened up to me about the exhaustion and, most painfully, the distance it was creating in his marriage. He felt his vitality had vanished. I shared my story and gave him an extra bottle.
Three months later, he pulled me aside with a grin I hadn't seen in years. "Robert... my energy is back. My wife is happy, and I'm happy. I feel like I've gotten a part of myself back that I thought was lost forever."
⭐⭐⭐⭐⭐ "My vitality has significantly improved"
"Besides supporting my prostate health, my overall energy and vitality have improved. My wife noticed the difference too! I feel more like my younger self."
— Frank L., 56, Arizona | ✓ Verified Buyer
Why am I sharing all this with you?
Because this isn't just my story. It's the story of real men who decided to try a different approach. And it could be your story, too.
If this supportive approach worked for us... why wouldn't you give yourself the chance to see what's possible?
With the 180-day guarantee, you have nothing to lose. But think of everything you have to gain:
✅ The possibility of more restful, peaceful nights.
✅ More energy and vitality to enjoy your day.
✅ The confidence to live life on your own terms.
✅ The chance to reconnect with the people you love.
The only question is: Are you ready to take the first step?
After my transformation, I couldn't keep quiet. Here's what happened next...
The ProstaVive Difference: An Engineer's Perspective
During my research, I learned to differentiate between a well-designed formula and a generic one. ProstaVive stood out for five logical reasons:
1. A Design Based on a Solid Principle
Instead of simply grouping together trendy ingredients, the formula is designed with a clear purpose: to support the fundamental mechanism of male well-being—the “internal hydraulics” fueled by healthy blood flow and nitric oxide production.
2. A Commitment to Quality Ingredients
The effectiveness of any system depends on the quality of its components. The formula uses ingredients from renowned sources, such as boron from Tibetan mineral deposits and Panax ginseng from the mountains of Manchuria, all tested to ensure purity and potency.
3. A Focus on Efficient Absorption
The formula comes in powder form, not capsules. The logic behind this is bioavailability. A liquid solution is designed to be efficiently absorbed by the body, ensuring that valuable nutrients are put to good use.
4. Rigorous Quality Control
The product is manufactured in a laboratory that follows international quality standards (GMP - Good Manufacturing Practices). For an engineer, this is non-negotiable. It means process control, consistency, and a product free of unnecessary additives or fillers.
5. A Philosophy of Synergy
This is not just a list of ingredients; it is a matrix. Each component is included in specific proportions, designed to work together. We believe that the combined effect of a synergistic formula is much greater than the sum of its individual parts.
An Important (and Honest) Note Before You Decide
Based on my experience and what I've heard from others, there is one practical drawback you need to be aware of: the supply of ProstaVive may be limited.
From what I understand, there are two reasons for this, both of which make sense from a quality standpoint:
1. Specific Ingredients: The formula relies on high-purity components, such as boron from Tibetan mineral deposits and pure Tongkat Ali from Southeast Asia. These are not mass-produced ingredients, and obtaining them consistently is a logistical challenge.
2. Small-Batch Production: To ensure maximum potency and quality, the lab produces ProstaVive in small, controlled batches, not on a giant assembly line.
The result is that demand, driven primarily by word of mouth, often outstrips production capacity. Some of the friends with whom I shared my story had to wait to place their orders.
The Good News for You Today
It seems you've arrived at a good time. While checking this page to make sure everything was still correct, I noticed that the company has a new batch in stock and is offering a significant discount for new customers, along with the 180-day guarantee that gave me the confidence to get started.
However, given the challenge of sourcing the ingredients and the small-batch production process, this stock probably won't last long. Once it sells out, there will likely be another waiting period.
So, if you're seriously considering taking this step, I honestly recommend securing your supply while it's available.
The Smart Choice I Made (And How You Can Too)
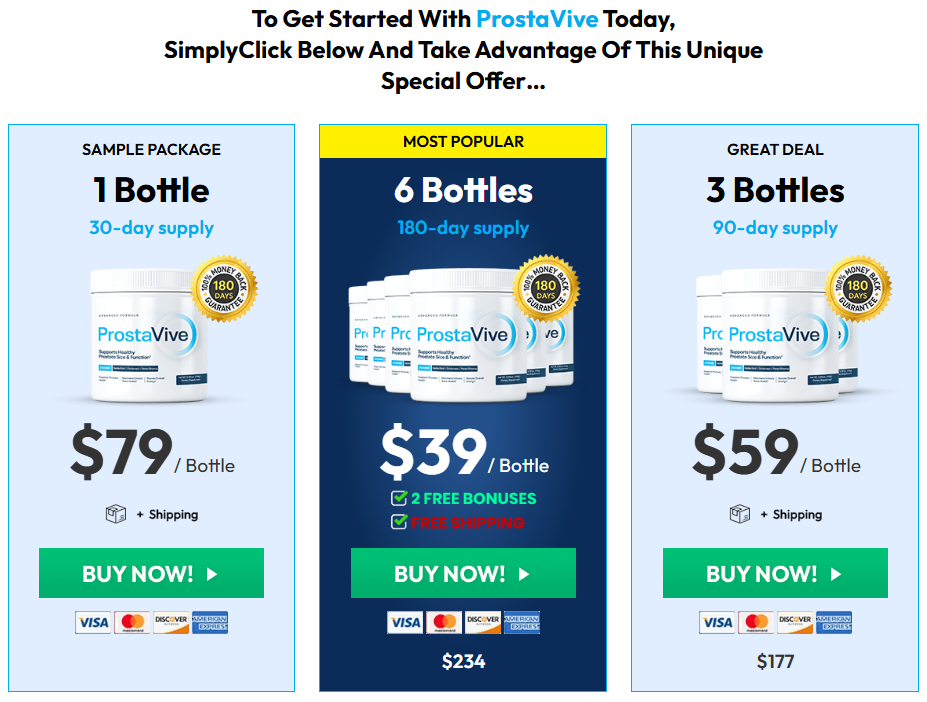
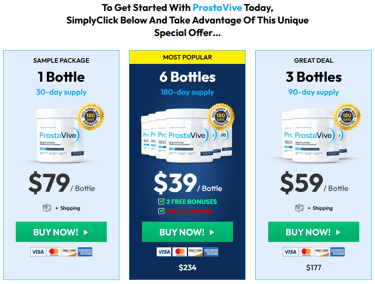
OPTION 1: 1 Bottle Package (30 days)
$79
1-month supply
180-day guarantee
OPTION 2: 3 Bottles Package (90 days) ⭐ BEST SELLER
$177
3-month supply
$59 per bottle
180-day guarantee
Free shipping
OPTION 3: 6 Bottles Package (180 days) 🏆 BEST VALUE
$234
6-month supply
$39 per bottle
180-day guarantee
Free shipping
Save $240
⚠️ MY PERSONAL LOGIC ON CHOOSING A PLAN:
As an engineer, I think in terms of systems. My body is a complex system, and I knew it would need time to respond to nutritional support. That's why I concluded that to give this a fair shot, I needed at least 90 days. For me, the 90 or 180-day option wasn't just the best value; it was the only logical way to conduct my "personal experiment."
The Guarantee That Made My Decision Risk-Free
Here’s what ultimately gave me the confidence to click the "buy" button: the company’s 180-day guarantee.
The terms were simple and direct: I had 6 full months to put ProstaVive to the test. If I didn't feel a noticeable improvement in my overall well-being, my daily energy, and my nightly comfort... or if I wasn't 100% satisfied for any reason at all... I could simply send an email to their support team and get 100% of my money back. No questions, no hassle. It removed all the risk from my decision.
The Choice I Realized I Had to Make
When I was at this crossroads, I laid out my options logically:
MY OPTION 1: Do Nothing.
Cost: $0 today.
My Risk: I knew the frustration would continue, and my quality of life would likely keep shrinking over time.
MY OPTION 2: Conventional Routes.
I had already spoken with my doctor, and I encourage you to do the same. Understanding all professional medical options is a responsible first step.
MY OPTION 3: Try This Proactive Nutritional Support.
Cost: Less than my daily cup of coffee.
My Risk: Zero. The company's 180-day guarantee meant I could get my money back if I wasn't satisfied.
My Opportunity: The chance to proactively support my body with smart nutrition, focused on the "flow support" mechanism I had researched.
For me, the choice became obvious.
I Know the Doubts You're Having, Because I Had Them Too
"Will this really work for me?"
This was my biggest question. What convinced me was that the formula wasn't just another mix of herbs. It was designed to support the fundamental mechanism of male "hydraulics"—healthy blood flow. The company's guarantee meant I didn't have to guess; I could find out for myself, risk-free.
"I've tried other supplements and they didn't work..."
I had too. I spent a small fortune on things that did nothing. The difference I saw here was the engineering philosophy: the synergy between the components and the singular focus on supporting flow, which my research pointed to as the root of the issue.
"It seems expensive..."
I'll admit, I also thought about the cost. But then I asked myself: What is a full night's sleep worth? What's the value of having the energy to play with my grandkids? For less than a daily coffee, I was making an investment in my quality of life. And I saw it as a temporary investment to support my system, not a lifelong bill.
"I'm embarrassed to order this..."
This is a private matter. I get it. I was relieved to see their packaging is 100% discreet. No one will know what's inside. You order online, from home, without any awkward conversations.
"But what if it doesn't work for me?"
This was my final thought, the one that sealed the deal. The absolute worst-case scenario was that I would send an email and get my money back thanks to the company's guarantee. I realized I had absolutely nothing to lose by trying.
Look, I'm going to be direct with you, just as I would be with a close friend.
From where I stand, you have a clear choice to make. It's the same choice I had to make eight months ago.
CHOICE 1: Do Nothing.
You can close this page and let today be just like yesterday. For me, that meant accepting the sleepless nights, the constant fatigue, the shrinking world, and the risk that nothing would ever change.
CHOICE 2: Take a Logical, Risk-Free Step.
You can do what I did: decide to give this a fair try. Give yourself 30, 60, or even 90 days to see what's possible for you.
See if you can experience:
The chance to enjoy deeper, more restful sleep.
The opportunity to feel more comfort and confidence throughout your day.
The possibility of reclaiming your energy and vitality.
The chance to reconnect with your loved ones without the strain of exhaustion.
The freedom to start living life on your own terms again.
And the logical backstop? If you don't feel a meaningful difference, the company's guarantee means you get a full refund.
For me, the choice was obvious.
A Final, Practical Thought From Me to You:
Based on my own experience when I first ordered and what I've heard from friends I've shared this with, the supply challenges are real. The high-quality ingredients and small-batch production mean it's often out of stock.
If you are leaning towards trying this, I would honestly suggest securing your supply from this current batch.
Don't wait. Click the button below and lock in your choice while it's still available.
Still in doubt? Remember my story.
Eight months ago, I was struggling. Waking up constantly. My energy was gone. My marriage was strained to the breaking point.
Today, I wake up feeling rested. My energy is back. I feel like myself again. My marriage is stronger than ever.
I can't promise you'll have my exact results. Nobody can. But I can tell you that taking that first step was the best decision I've made for my well-being in years.
And you're not really risking anything to find out. The company's 180-day guarantee protects you completely.
You truly have nothing to lose, and the possibility of everything to gain.
Privacy Policy | Terms & Conditions | Contact Us
Product & Order Support:
For questions about the product, please contact: support@prostavive.org or (863) 591-4284.
For questions about your order, please contact our retailer ClickBank HERE.
IMPORTANT DISCLAIMERS:
This product is a dietary supplement and is not intended to diagnose, treat, cure, or prevent any disease. The statements made on this website have not been evaluated by the Food and Drug Administration.
The information provided on this site is for educational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. Always consult your physician before starting any supplementation program, especially if you have underlying health conditions or are taking medications.
Individual results may vary. The testimonials presented are real customer experiences but do not guarantee that you will have the same results.
ClickBank Disclaimer:
ClickBank is the retailer of products on this site. CLICKBANK® is a registered trademark of Click Sales Inc., a Delaware corporation located at 1444 S. Entertainment Ave., Suite 400, Boise, ID 83709, USA and used by permission. ClickBank's role as retailer does not constitute an endorsement, approval or review of these products or any claim, statement or opinion used in promotion of these products.
© 2025 CMF. All Rights Reserved.